Back Lower or Upper Pain Control with or without Bulging Lumbar Discs >>
CORE SUPPORT PROGRAM >>
Tendon Mender one cap twice per day
Joint Performance two softgels twice per day
ArthritX two softgels twice per day
CollagenMAX one cap twice per day
Inflam-X three to four caps twice per day
Cell Defense PLUS two caps twice per day
Red Deer Velvet DR three to fou rcaps twice per day NADH two tabs under tongue four times per day HGH Spray four sprays under four times per day Joint Connective Tissue and Vascular Peptides one twice per day month one, then taken at supper times
Omega Supreme Pro two softgels twice per day
Topical Therapies >>
PAINAWAY CREAM apply to regions of pain every two to four hours during the day
ADVANCED PROTOCOLS >>
CALMind one scoop two to three times per day in drink
Brain Mag one scoop two to three time per day in drink
Sphilkes one to two caps muscle relaxant two to three times per day
NeuroGEN two softgels twice per day
POWER C Plus two to three caps twice per day
Full Vitamin K2 one cap twice per day
Minerals PLUS and VitaMineralMAX one cap each twice per day
SonicLife Whole Body Resistance Bank and Peptide Frequency Therapies twice per day 10 minutes
https://www.nutrimedical.com/product-category/soniclife-sound-emf-exercise-healing-field-therapy/
Lumen Photon Setting 7 for Pain and NICO for spinal healing over regions of pain
https://www.nutrimedical.com/product-category/lumen-photon/
Back pain and sciatica – Symptoms and Causes
and Description
An in-depth report on the causes, diagnosis, treatment, and prevention of back pain, including sciatica.
Alternative Names
Herniated disk; Sciatica
Symptoms and Causes:
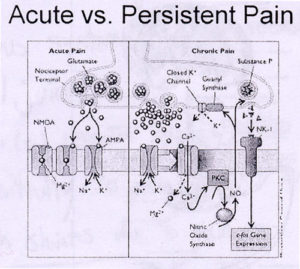
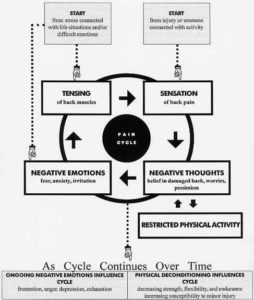
The origin of the pain is often unknown, and imaging studies may fail to determine its cause. Disk disease, spinal arthritis, and muscle spasms are the most common diagnoses. Other problems can also cause back pain, however.
Muscle and Ligament Injuries/Lumbar Strain
Strain and injury to the muscles and ligaments supporting the back are the major causes of low back pain. The pain is typically more spread out in the muscles next to the spine, and may be associated with spasms in those muscles. The pain may move to the buttocks but rarely any farther down the leg.
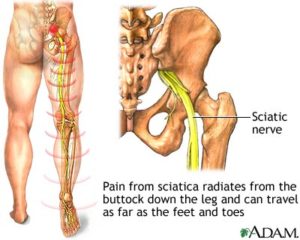
Sciatica
The sciatic nerve is a large nerve that starts in the lower back.
It forms near the spine and is made up from branches of the roots of the lumbar spinal nerves.
It travels through the pelvis and then deep into each buttock.
It then travels down each leg. It is the longest and widest single nerve in the body.
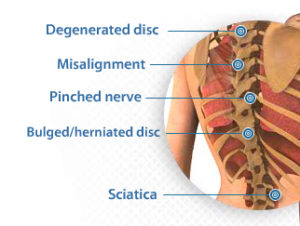
Sciatica is not a diagnosis but a description of symptoms. Anything that places pressure on one or more of the lumbar nerve roots can cause pain in parts or all of the sciatic nerve. A herniated disk, spinal stenosis, degenerative disc disease, spondylolisthesis, or other abnormalities of vertebrae can all cause pressure on the sciatic nerve.
Some cases of sciatica pain may occur when a muscle located deep in the buttocks pinches the sciatic nerve. This muscle is called the piriformis. The resulting condition is called piriformis syndrome. Piriformis syndrome usually develops after an injury. It is sometimes difficult to diagnose.
The main nerve traveling down the leg is the sciatic nerve. Pain associated with the sciatic nerve usually originates when nerve roots in the spinal cord become compressed or damaged. Symptoms can include tingling, numbness, or pain that radiates to the buttocks, legs, and feet.
Sciatic nerve
Pain or numbness due to sciatica can vary widely. It may feel like a mild tingling, dull ache, or a burning sensation. In some cases, the pain is severe enough to cause immobility.
The pain most often occurs on one side and may radiate to the buttocks, legs, and feet. Some people have sharp pain in one part of the leg or hip and numbness in other parts. The affected leg may feel weak.
The pain often starts slowly. Sciatica pain may get worse:
At night
After standing or sitting for long periods of time
When sneezing, coughing, or laughing
After bending backwards or walking more than 50 – 100 yards (particularly if it is caused by spinal stenosis — see below)
Sciatica pain usually goes away within 6 weeks, unless there are serious underlying conditions. Pain that lasts longer than 30 days, or gets worse with sitting, coughing, sneezing, or straining may indicated a longer recovery. Depending on the cause of the sciatica, symptoms may come and go.
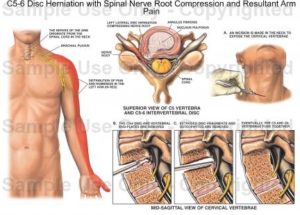
Herniated Disk
A herniated disk, sometimes (incorrectly) called a slipped disk, is a common cause of severe back pain and sciatica. A disk in the lumbar area becomes herniated when it ruptures or thins out, and degenerates to the point that the gel within the disk (the nucleus pulposus) pushes outward. The damaged disk can take on many forms:
A bulge — The gel has been pushed out slightly from the disk and is evenly distributed around the circumference.
Protrusion — The gel has pushed out slightly and asymmetrically in different places.
Extrusion — The gel balloons extensively into the area outside the vertebrae or breaks off from the disk.
Pain in the leg may be worse than the back pain in cases of herniated disks. There is also some debate about how pain develops from a herniated disk and how frequently it causes low back pain. Many people have disks that bulge or protrude and do not suffer back pain. Extrusion (which is less common than the other two conditions) is highly associated with back pain, since the gel is likely to extend out far enough to press against the nerve root, most often the sciatic nerve. Extrusion is very uncommon, however, while sciatic and low-back pain are very common. But there may be other causes of low back pain.
Abnormalities in the Annular Ring. Research has also focused on tears in the annular ring — the fibrous band that surrounds and protects the disk. The annular ring contains a dense nerve network and high levels of peptides that heighten perception of pain. Tears in the annular ring are a frequent finding in patients with degenerative disk disease. Some cases of chronic low back pain may be caused by inward growth of nerve fibers into the annular ring, which triggers pain within the intervertebral disk.
Cauda equina syndrome. Cauda equina syndrome is the impingement of the cauda equina (the four strands of nerves leading through the lowest part of the spine). The cause is usually massive extrusion of the disk material. Cauda equina syndrome is an emergency condition that can cause severe complications to bowel or bladder function. It can cause permanent incontinence if not promptly treated with surgery. Symptoms of the cauda equina syndrome include:
Dull back pain
Weakness or numbness in the buttocks, in the area between the legs, or in the inner thigh, backs of legs, or feet; may cause stumbling or difficulty in standing
An inability to control urination and defecation
Pain accompanied by fever (can indicate an infection)
Lumbar Degenerative Disk Disease/Spondylosis
Osteoarthritis occurs in joints of the spine, usually as a result of aging, but also in response to previous back injuries, excessive wear and tear, previously herniated discs, prior surgeries, and fractures. Cartilage between the joints of the spine is destroyed and extra bone growth or bone spurs develop. The rate at which these changes develop varies between people.. The end result of these changes is a gradual loss of mobility of the spine, narrowing of the spaces for spinal nerves and spinal cord, and drying out or degeneration of the spinal discs. Depending on which part and how much of the spine is involved, symptoms may be similar to that of a herniated disc, lumbar strain, or spinal stenosis (narrowing of the spinal canal).
Spinal Stenosis
Spinal stenosis is the narrowing of the spinal canal, or narrowing of the openings (called neural foramina) where spinal nerves leave the spinal column. This condition typically develops as a person ages and the disks become drier and start to shrink. At the same time, the bones and ligaments of the spine swell or grow larger due to arthritis and chronic inflammation. However, other problems, including infection and birth defects, can sometimes cause spinal stenosis.
Most patients will report the presence of gradually worsening history of back pain over time. For others, there may be minimal history of back pain, but at some point in this process any disruption, such as a minor injury that results in disk inflammation, can cause impingement on the nerve root and trigger pain.
Patients may experience pain or numbness, which can occur in both legs, or on just one side. Other symptoms include a feeling of weakness or heaviness in the buttocks or legs. Symptoms are usually present or will worsen only when the person is standing or walking upright. Often the symptoms will ease or disappear when sitting down or leaning forward. These positions may create more space in the spinal canal, thus relieving pressure on the spinal cord or the spinal nerves. Patients with spinal stenosis are not usually able to walk for long periods of time. They may be able to ride an exercise bike.
Spondylolisthesis
Spondylolisthesis occurs when one of the lumbar vertebrae slips over another, or over the sacrum.
In children, spondylolisthesis usually occurs between the fifth bone in the lower back (lumbar vertebra) and the first bone in the sacrum area. It is often due to a birth defect in that area of the spine. In adults, the most common cause is degenerative disease (such as arthritis). The slip usually occurs between the fourth and fifth lumbar vertebrae. It is more common in adults over 65 and women.
Other causes of spondylolisthesis include stress fractures (commonly seen in gymnasts) and traumatic fractures. Spondylolisthesis may occasionally be associated with bone diseases.
Spondylolisthesis may vary from mild to severe. It can produce increased lordosis (swayback), but in later stages may result in kyphosis (roundback) as the upper spine falls off the lower spine.
Symptoms may include:
Lower back pain
Pain in the thighs and buttocks
Stiffness
Muscle tightness
Tenderness in the slipped area
Pain generally occurs with activity and is better with rest. Neurological damage (leg weakness or changes in sensation) may result from pressure on nerve roots, and may cause pain radiating down the legs.
Inflammatory Conditions and Arthritis
Inflammatory disorders and arthritis syndromes can produce inflammation in the spine.
Ankylosing spondylitis is a chronic inflammation of the spine that may gradually result in a fusion of vertebrae. Symptoms include a slow development of back discomfort, with pain lasting for more than 3 months. The back is usually stiff in the morning; pain improves with movement or exercise. In severe cases, the patient stands or sits stooped over. It can be quite mild, however, and it rarely affects a person’s ability to work. It occurs mostly in young Caucasians in their mid-20s. The disease is more common in men, but about 30% of the cases are in women. Researchers believe that in most cases the cause is hereditary.
About 20% of people with inflammatory bowel disease and about 20% of people with psoriasis develop a similar form of arthritis involving the spine. There are multiple treatments for this potentially disabling disease, including various immune suppressant medications. Etanercept (Enbrel) and infliximab (Remicade), anti-inflammatory agents known as TNF-blockers, are proving to be beneficial.
Osteoporosis and Compression Fractures
Osteoporosis is a disease of the skeleton in which the amount of calcium present in the bones slowly decreases to the point where the bones become fragile and prone to fractures. It usually does not cause pain unless the vertebrae collapse suddenly, in which case the pain is often severe. More than one vertebra may be affected.
In a compression fracture of the vertebrae, the bone tissue of the vertebra collapses. More than one vertebra may collapse as a result. When the fracture is the result of osteoporosis, the vertebrae in the thoracic (chest) and lower spine are usually affected, and symptoms may be worse with walking.
With multiple fractures, kyphosis (a forward hump-like curvature of the spine) may result. In addition, compression fractures are often responsible for loss of height. Pressure on the spinal cord may also occur, producing symptoms of numbness, tingling, or weakness. Symptoms depend upon the area of the back that is affected; however, most fractures are stable and do not produce neurological symptoms. [For more information, see In-Depth Report #18: Osteoporosis.]
Back Pain Emergencies
Several serious conditions can also cause back pain. Often, these symptoms develop over a short period of time, become more severe, and may have other findings that go along with them. Some of these conditions include:
Infection in the bone (osteomyelitis) or the disk (diskitis)
Cancer that has spread to the spine from another part of the body (most commonly lung cancer, colon cancer, prostate cancer, and breast cancer)
Cancer that begins in the bones (the most common diagnosis in adults is probably multiple myeloma, seen in middle age or older adults); benign tumors such as osteoblastoma or neurofibroma and cancers, including leukemia, can also cause back pain in children
Trauma
Miscellaneous Abnormalities and Diagnoses
Any abnormality in joints, vertebrae, or nerve roots can cause back pain, including:
Fibromyalgia.
Other medical conditions that cause referred back pain, occurring in conjunction with problems in organs unrelated to the spine (although usually located near it); such conditions include ulcers, kidney disease (including kidney stones), ovarian cysts, and pancreatitis.
Chronic uterine or pelvic infections can cause low back pain in women.
The facet joints (z-joints) can wear down; in such cases, pain occurs on arching the back or when walking.
In some cases a segment (consisting of two vertebrae and their common joint and disk) becomes unstable when its parts wear down.
Injury to nerve roots, notably deep root ganglia (nerve cells in the spine whose fibers extend from skin to muscle tissue), may be important in some cases; some patients may have scar tissue that traps the nerve roots in the lower spine and causes sciatica.
Resources
www.niams.nih.gov — National Institute of Arthritis and Musculoskeletal and Skin Diseases
www.aaos.org — American Academy of Orthopaedic Surgeons
www.arthritis.org — Arthritis Foundation
www.spine.org — North American Spine Society
www.apta.org — American Physical Therapy Association
www.ampainsoc.org — American Pain Society
www.theacpa.org — American Chronic Pain Association
www.iasp-pain.org — International Association for the Study of Pain
Disclaimer: These Wellness Protocols are not intended to replace the attention or advice of a physician or other qualified healthcare professional. These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure, or prevent any disease.