MULTIPLE SCLEROSIS and TRANSVERSE MYELITIS RECOVERY WELLNESS PROTOCOLS >>
Remyelination Multiple Sclerosis Protocol:
Cell Defense
Power C PLUS
Red Deer Velvet DR
Sphingolin
CoQ10 Supreme Ubiquinol
Ultra Thiamine B1
Mega Muscles
Gamma E Plus
CALMIND
Cell Detox Glutathione
Selenium Cruciferate
My Cell D3
NeuroGEN
ADVANCED>>>>
Omega Supreme Pro
Power Methyl B12
Super Folate TR
VitaMineralMAX
NADH
Mitochondrial Energy
Nutriodine
AllicinMED
NutriDefense
KardioVasc
SuperNOX Plus NO2 Beets
Brain Power
Cognition PLUS one cap three times per day
Brain Peptides and Vascular Peptides
Lumen Photon to sides and back of head Frequency 3 for 30 minutes three times per day, 180 pad with velcro and under pillow with sleep
DIET – Allergen, Glutamate, Gluten FREE Diet – Alkalinizing Ketogenic Diet

7492-Facts-Stats-MS
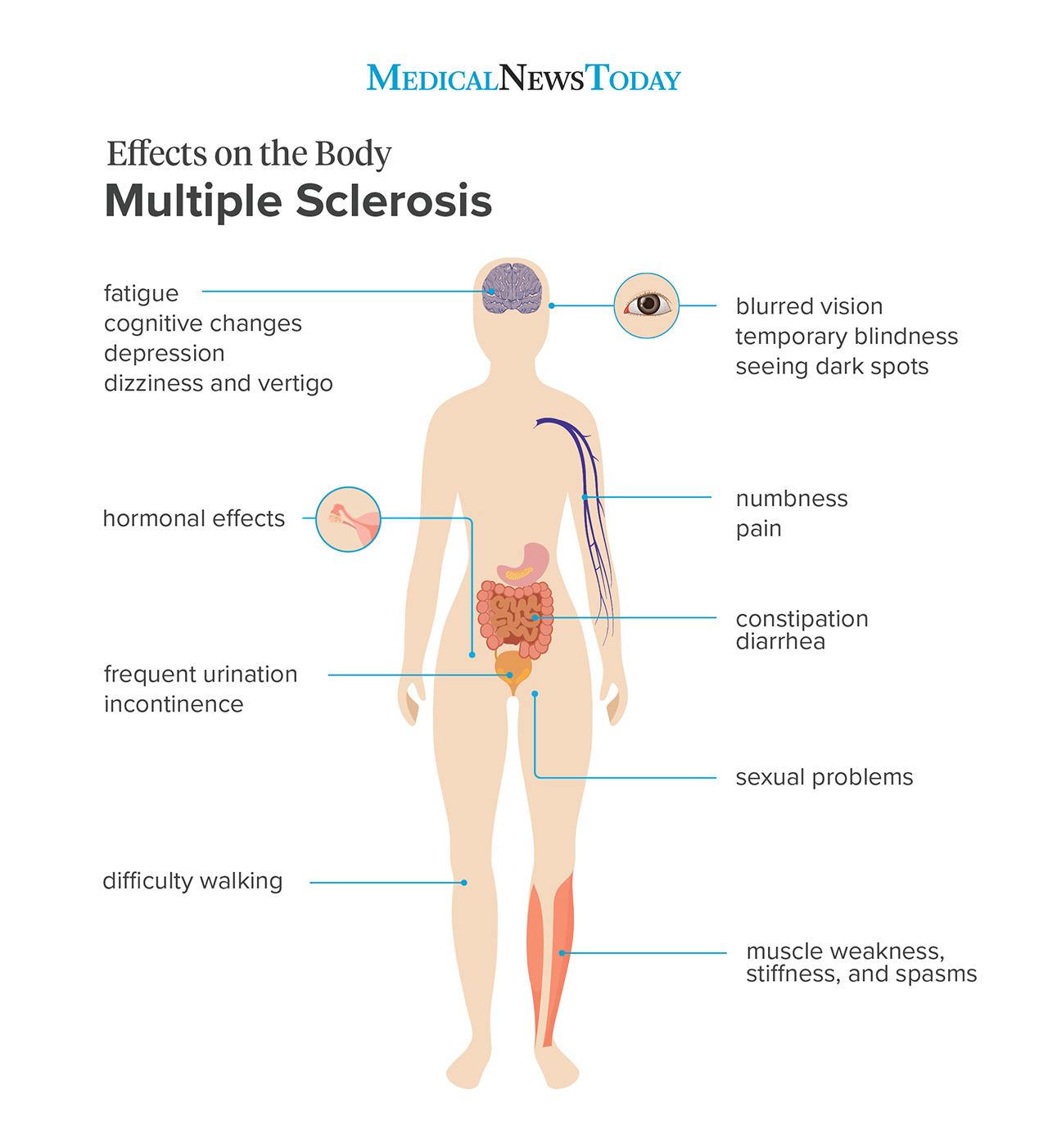
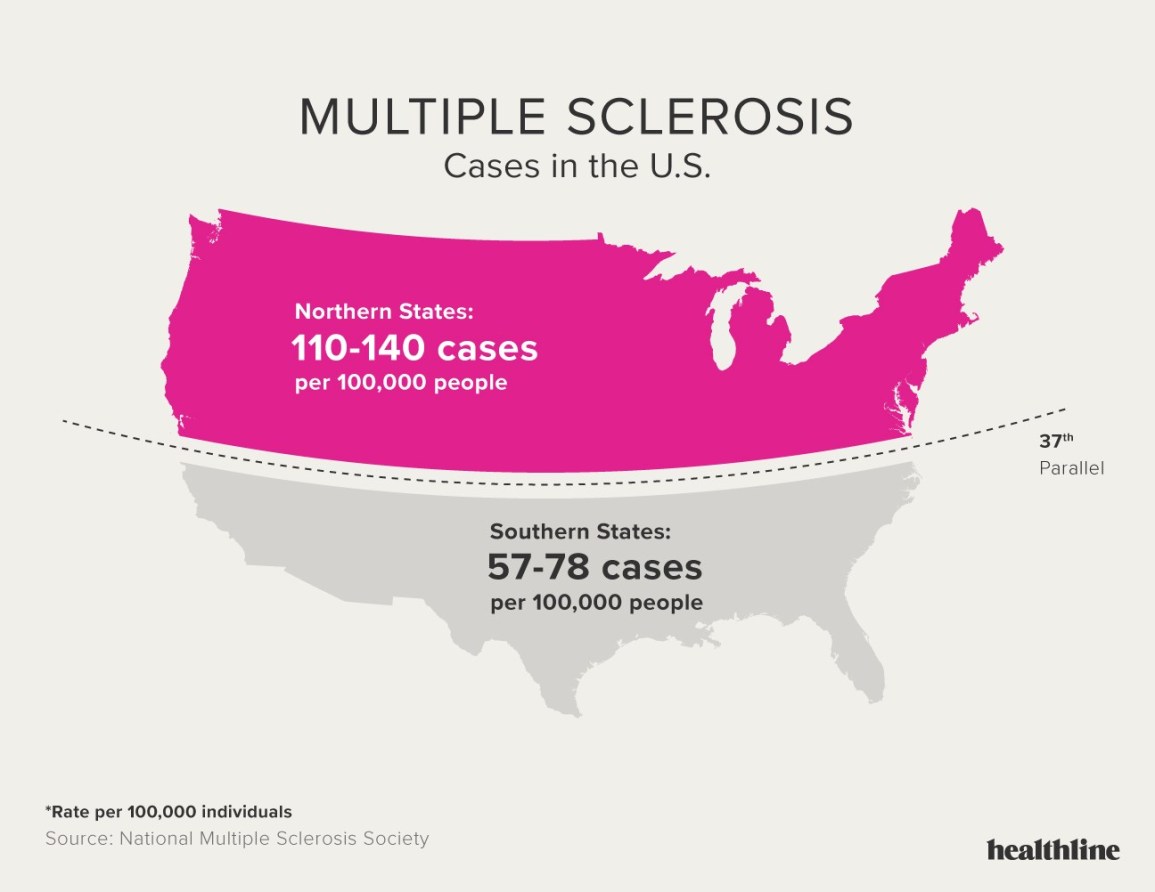
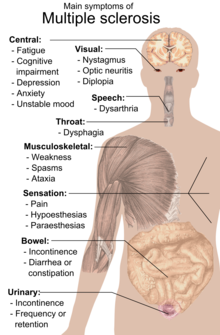
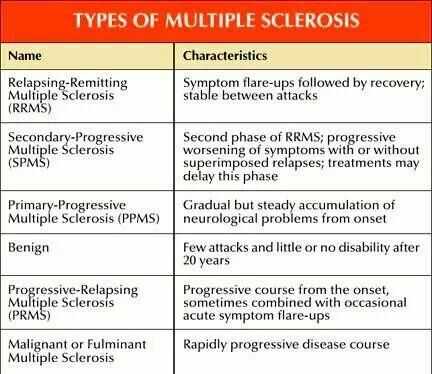
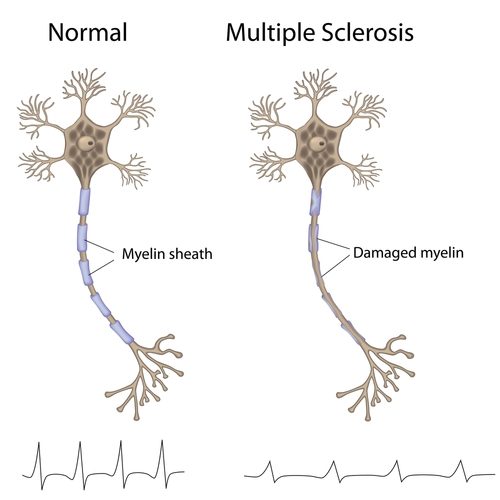
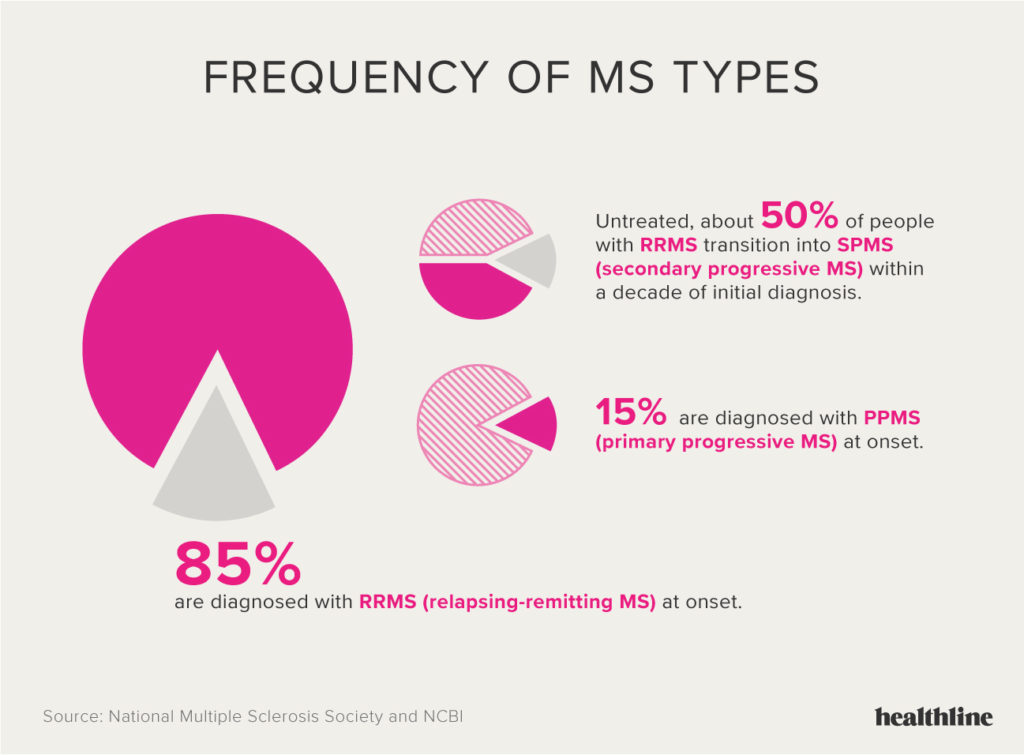
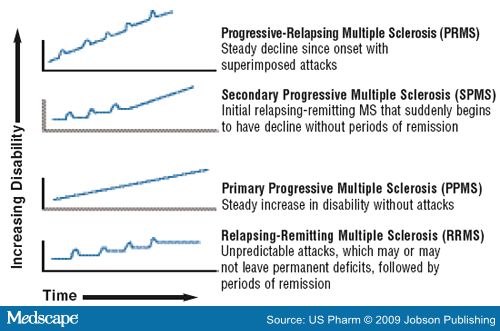
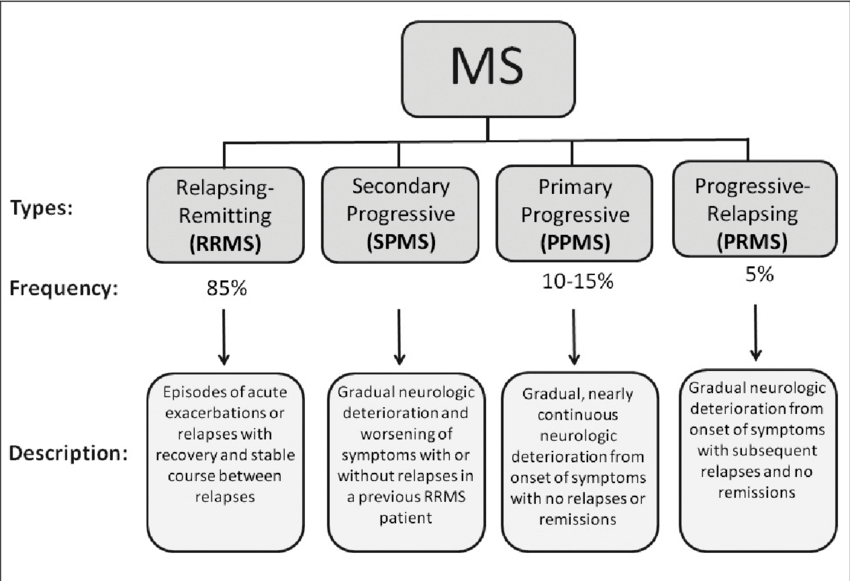
Multiple sclerosis (MS) is a syndrome of chronic nerve disturbances due to a process called demyelination, a gradual loss of the myelin sheath surrounding each nerve cell. The myelin sheath plays an essential role in transmission of the nerve impulse. Without the myelin sheath, nerve transmission cannot occur, so nerve function is lost. Symptoms correspond to this loss of function in the affected nerves. Incidence of MS follows a geographic distribution with areas of highest frequency all located in the higher latitudes, in both the northern and southern hemispheres (50–100 cases per 100,000 in higher latitudes versus 5–10 cases per 100,000 in the tropics). High-risk areas include the northern US, Canada, Great Britain, Scandinavia, northern Europe, New Zealand, and Tasmania. It also appears that the initiating event in MS may occur early in life since people who move from a low risk to a high-risk area before the age of 15 have a higher risk of developing MS, while those who make the same move after age 15 retain their lower risk. In about two-thirds of cases, onset is between the ages of 20–40 years, and women are more frequently affected than men – incidence is 60% female to 40% male. The rate of progression varies considerably in MS. One-third of patients have mild, non-progressive disease; one-third worsen slowly; and one-third worsen rapidly. FREQUENT SIGNS AND SYMPTOMS Initial symptoms may occur alone or in combination. Typically, symptoms develop over a few days or weeks, recede, then recur. Early stages Sudden transient motor and sensory disturbances including:
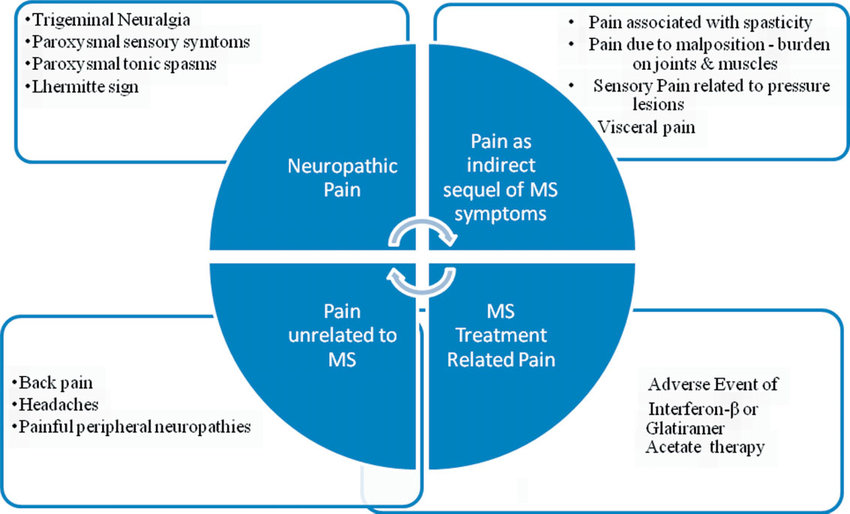
• intermittent blurred or double vision, fogginess, haziness, eyeball pain or other vague eye problems
• muscle weakness
• feeling of heaviness, leg dragging, stiffness
• tendency to drop things, clumsiness
• dizziness, light-headedness, feeling of spinning, sensation of drunkenness, nausea, vomiting
• difficulty with walking or balance
• vague loss of sensation
• tingling “pins and needles” sensation, numbness, band-like tightness, electrical sensations Laboratory findings
• Elevated IgG antibodies in cerebrospinal fluid: found in 80–90% of patients with MS, although also present in other neurological conditions
• Nerve function assessment (evoked-potential studies): abnormalities found in 94% of patients with established MS, and 67% of patients with suspected MS
• Magnetic resonance imaging (MRI) showing demyelination in the nervous system
• Excessive platelet adhesiveness (stickiness)
• Decreased levels of omega-3 essential fatty acids in the serum, erythrocytes, and cerebrospinal fluid Late stages
• Marked muscular weakness and tremor
• Difficulty speaking
• Loss of bladder sensation, bladder or bowel control
• Extreme mood swings
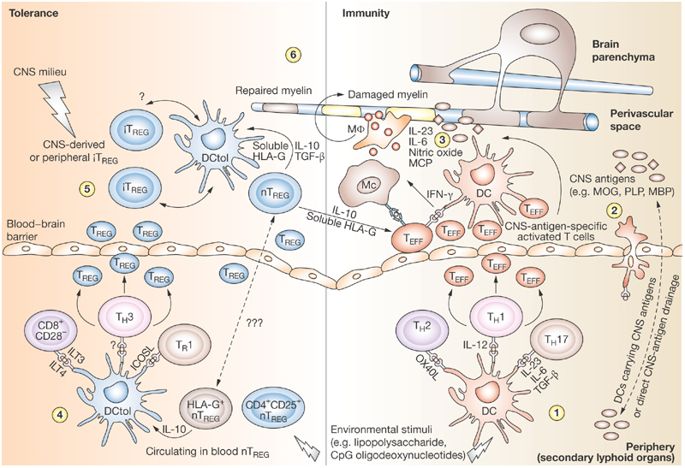
• Sexual impotence in men CAUSES The cause(s) of MS remain to be identified conclusively. Numerous causative factors have been proposed including the following. • Viral infection: viruses are known to cause several demyelinating diseases similar to MS in humans and animals, and studies have demonstrated that viruses can cause demyelination either by directly damaging the myelin-producing cells or by prompting an immune response in which antibodies are formed that attack the myelin:
• a number of viruses have been identified in patients with MS including rabies virus, herpes simplex virus, scrapie virus, parainfluenza virus, subacute myelo-opticoneuropathy virus, coronavirus, and measles virus.
• measles is the most suspicious potential cause of MS, although recent studies have shown that the measles-specific antibody in MS patients accounts for only a small percentage of their total antibody level.
• the cerebrospinal fluid (the fluid surrounding the brain and spinal cord) of most MS patients contains an elevated level of IgG antibodies (proteins made by the immune system’s white blood cells that bind to alien molecules such as bacteria, viruses, and cancer cells) in a pattern characteristic of an immune response to an infectious process.
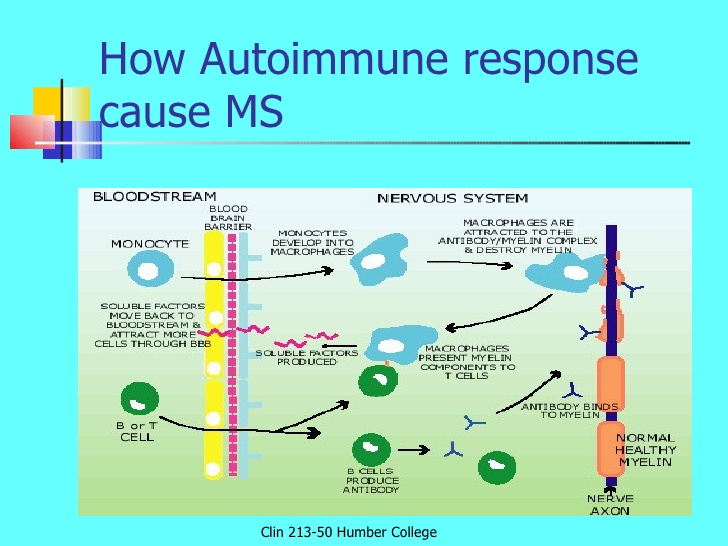
• at present, however, available data do not suggest a common virus is the cause for these increased IgG antibody levels; they are thought to result from an autoimmune reaction. • Autoimmune reaction: the lesions in the nerve cells of MS patients are similar to those produced in animals after injecting them with myelin:
• the autoimmune disease produced in animals (experimental allergic encephalomyelitis) is the result of the animals’ reaction to a single antigen (myelin basic protein).
• humans with MS show no evidence of an increase in antibody levels to myelin basic protein. Considerable evidence suggests that MS is an autoimmune disease, but it must be due to some other antigen. • Excessive lipid peroxidation: patients with MS frequently are found to have reduced levels or activity of a very important antioxidant enzyme called glutathione peroxidase:
• glutathione peroxidase (GSH-Px) is critical for the protection of cells from free radicals. Decreased levels or activity of GSH-Px render the myelin sheath much more susceptible to damage. The myelin sheath is largely composed of fats (lipids), so when it is damaged (oxidized) by free radicals, lipid peroxides are formed.
• GSH-Px is found in two enzymatic forms: selenium dependent and non-selenium dependent.
• decreased levels of selenium-dependent GSH-Px are most probably the result of inadequate amounts of selenium in the diet. Areas in which selenium levels in the soil are low often overlap areas in which incidence of MS is high.
• reduced activity of GSH-Px in MS patients is most likely the result of genetic factors: MS incidence is higher in individuals with a form of GSH-Px with low activity (GSH-PxL), compared to individuals genetically endowed with a form of GSH-Px with high activity (GSH-PxH). • Pro-inflammatory diet: a higher prevalence of MS has been correlated with diets high in animal and dairy products, especially when compared to diets high in cold-water fish:
• inland farming communities in Norway, in which animal products comprise a large portion of the diet, have a higher incidence of MS than areas near the coastline where fish is a primary protein source.
• in Japan, despite its northern latitude, MS incidence is quite low, and the traditional Japanese diet is also high in seafood, along with seeds and soyfoods.
• domestically grown animal and dairy products contain high amounts of arachidonic acid, while fish, seeds and soyfoods are abundant in the omega-3 oils (alpha-linolenic, eicosapentaenoic, and docosahexanoic acids):
• arachidonic acid is metabolized in the body to produce series 2 prostaglandins, which promote inflammation.
• omega-3 fats are metabolized in the body to produce series 1 and 3 prostaglandins, both of which are anti-inflammatory.
• deficiencies of these omega-3 oils interfere with the elongation of fats that compose nerve cell membranes and permanently impair formation of normal myelin.
• the epidemiological data suggest that disease results when consumption of animal fats, our primary source of pro-inflammatory arachidonic acid, is not balanced by comparable consumption of the anti-inflammatory omega-3 fats found in fish, seeds, and soy foods.
• a diet low in omega-3 fats may be a significant factor in patients with MS:
• normal myelin is largely composed of omega-3 fats.
• omega-3 fats decrease both the platelet aggregation (clumping together) seen in atherosclerosis as well as MS, and the autoimmune response in which the immune system attacks the myelin sheath.
• excessive platelet aggregation and very small clumps of platelets (microemboli) are thought to damage the blood-brain barrier, and cause alterations in the microcirculation of the central nervous system, and reduced blood flow to the brain seen in MS.
• damage to the blood–brain barrier allows passage of blood components toxic to myelin (bacteria, viruses, antibodies, toxic chemicals) into the cerebrospinal fluid.
• reduced blood flow to the brain promotes cellular death via the release of self-destructing enzymes, which can also destroy myelin. • Food allergy: consumption of two common allergens – gluten (found in wheat and other grains) and cow’s milk – has been implicated in MS:
• diets high in gluten and milk are much more common in areas in which prevalence of MS is high.
• intestinal biopsy of MS patients has shown increased frequency of significant damage to the intestinal lining similar to that which occurs in celiac disease and food allergies. RISK INCREASES WITH • Children and adolescents raised in northern latitudes.
• High intake of animal products, particularly when comparable intake of fish, seeds and soyfoods is lacking.
• Inadequate intake of selenium results in low levels of GSH-Px.
• Family history of MS: genetic susceptibility; low activity of GSH-Px. • Food allergy, especially to gluten and milk. • Use of non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, indometacin, etc.:
• NSAIDs inhibit the synthesis of prostaglandins from essential fatty acids. The prostaglandins formed from omega-3 fats reduce the autoimmune response, thus lessening the destruction of myelin.
• individuals with or at risk for MS should avoid NSAIDs. PREVENTIVE MEASURES • Ensure adequate intake of selenium:
• in addition to being needed for the seleniumdependent form of GSH-Px, selenium helps disarm free radicals formed from the arachidonic acid cascade and from a defensive tactic of the immune system (the phagocytic respiratory burst).
• best sources of selenium are seafood and meats. Meat consumption should, however, be minimized since meat is also the primary source of arachidonic acid.
• best plant sources of selenium include wheat germ, Brazil nuts, apple cider vinegar, red Swiss chard, and oats:
• the soil content of selenium will determine the amount found in plant sources. Plants grown in low-selenium areas cannot, therefore, be relied upon to supply standard amounts.
• recommended daily allowances (q.d.) for selenium are:
• children: 1–6 years, 20 ?g; 7–10 years, 30 ?g.
• males: 11–14 years, 40 ?g; 15–18 years, 50 ?g; 19??years, 70 ?g.
• females: 11–14 years, 45 ?g; 15–18 years, 50 ?g; 19+ years, 65 ?g. • Identify and eliminate food allergens: wheat and dairy should be prime suspects. • Ensure adequate intake of omega-3 oils by increasing intake of the foods richest in these oils:
cold-water fish, nuts (especially walnuts) and seeds (especially flaxseed, discussed below). • Increase intake of soyfoods: a good source of protein that compares favourably with beef, but without the high levels of fat found in most animal foods, soy also contains antioxidant phytochemicals, fiber, and polyunsaturated fats, including omega-3 oils. Expected outcomes • Individuals with minimal disability respond better than those with severe disability.
• Treatment including diet, lifestyle modification and supplementation should begin as soon as possible since the earlier in the disease process that treatment is initiated, the better the results.
• Normalization of red blood cell fatty acid levels requires a minimum of 2 years of supplementation. Since myelin-producing cells have a much longer half life than red blood cells, it could take several years before the total benefits of treatment will be observed.
• Once MS has progressed to significant disability, it is unlikely to be greatly affected by the natural therapies recommended below. Regardless of the progression of MS, these measures will, at the very least, provide the benefit of decreasing risk for atherosclerosis and other degenerative diseases. TREATMENT Lifestyle
Avoid excessive fatigue, emotional stress, and marked temperature changes. Diet
• The Swank diet: Dr Roy Swank, Professor of Neurology at the University of Oregon Medical School, who began successfully treating MS patients with a low animal fat diet in 1948, has provided convincing evidence that such a diet, maintained over a long period of time, reduces the number of attacks and retards the progression of MS.
• Swank’s diet effectively reduces the intake of arachidonic acid while increasing intake of essential fatty acids, particularly the omega-3 fats, which prevent platelet aggregation and are required for normal myelin composition (see Causes above).
• The Swank diet recommends:
• an intake of saturated fat of no more than 10 g q.d.
• daily intake of 40–50 g of polyunsaturated oils q.d.
• no margarine, shortening or hydrogenated oils
• at least 1 tsp of cod liver oil q.d.
• normal allowance of protein:
• a diet low in saturated fats significantly restricts animal protein.
• protein should be primarily derived from fish, legumes, grains, and vegetables.
• cold-water fish are preferred because of their excellent omega-3 as well as protein content and should be eaten three or more times per week.
• Food allergens should be identified and eliminated from the diet: wheat and dairy products are the most
• common allergens in patients with MS.
• Fresh whole foods should be emphasized and consumption of animal foods (with the exception of coldwater fish) should be reduced, if not completely eliminated. Nutritional supplements • A high-potency multiple vitamin and mineral supplement: a daily multiple providing all of the known vitamins and minerals serves as a foundation upon which to build an individualized health promotion program. Any good multiple should include 400 ?g of folic acid, 400 ?g of vitamin B12, and 50–100 mg of vitamin B6. (Folic acid supplementation should always be accompanied by vitamin B12 supplementation to prevent folic acid from masking a vitamin B12 deficiency.) • Flaxseed oil: flaxseed oil contains both linoleic (an omega-6 essential fatty acid) and alpha-linolenic acid (an omega-3 essential fatty acid):
• linoleic acid has been shown to greatly inhibit the progression of less severe forms of an autoimmune
• disease (experimental allergic encephalomyelitis) induced in animals by immunization with myelin.
• in several double-blind trials in patients with MS, similar beneficial effects have been seen. Supplementation with linoleic acid has resulted in a smaller increase in disability, and reduced severity and duration of relapses, compared with controls.
• as in animals, individuals with minimal disability respond better than those with severe disability. • Selenium: one form of the critically important antioxidant glutathione peroxidase (GSH-Px, discussed
• above) is selenium dependent:
• GSH-Px protects lipids (fats) from oxidation by free radicals.
• the membranes of cells, including nerve cells, are primarily composed of fats, as is the myelin sheath. • Vitamin E: a fat-soluble antioxidant, vitamin E, which works with selenium, provides the body’s primary defense against oxidative damage to all its lipid-rich constituents, including the cell membranes and myelin sheath of nerve cells:
• one study reported that supplementation of 18 MS patients with high dosages of selenium, vitamin E and vitamin C for 5 weeks increased GSH-Px levels fivefold. • Vitamin B12: both inborn errors of metabolism involving B12 and acquired B12 deficiency are well known causes of demyelination of nerve fibers in the central nervous system (CNS):
• in MS patients, vitamin B12 levels have been found to be low in serum, red blood cells and the CNS.
• a B12 deficiency may aggravate MS or promote another cause of progressive demyelination.
• in one recent study, researchers found that although the level of B12 in the serum of MS patients was normal, B12 was not getting into their cells, indicating a defect in the transport of the vitamin into cells:
• oral administration of 60 mg q.d. of B12 in the form of methylcobalamin – the main and most active form of B12 in the body, and the form directly related to the function of B12 in methylation reactions – improved both sight and hearing by nearly 30%.
• motor function did not improve, indicating that pathways to the brain benefit from B12, while those from the brain do not.
• these results are equivalent to those produced by cyclophosphamide (a very potent immunesuppressing
• drug) plus steroids – a combination associated with profound immune suppression and toxicity.
• no toxic side effects have been attributed to high doses of B12. • Pancreatin: in MS, as in other autoimmune diseases, levels of circulating immune complexes (antigens
• bound by antibodies) are abnormally high. Proteindigesting enzyme preparations (e.g., pancreatic extracts, bromelain, papain) have been shown to reduce these high levels:
• in MS, pancreatic enzyme preparations have been found to produce good effects in reducing severity and frequency of symptom flare-ups including visual disturbances, sensory disturbances, and urinary, bladder and intestinal malfunction. Little effect, however, has been noted on spasticity, dizziness, or tremor.
• many individuals with MS have some degree of malabsorption:
• in one study, 42% of MS patients had fat malabsorption, 42% had protein malabsorption, 27% had abnormal sugar absorption, and 12% had abnormal B12 absorption.
• pancreatic enzymes may also improve absorption. Botanical medicines
• Ginkgo biloba extract (GBE): in MS, increased levels of lipid peroxides and other indicators of free radical damage in the central nervous system suggest the need for antioxidant support:
• in numerous studies, GBE has demonstrated impressive antioxidant effects, and also lessens platelet aggregation, improves blood flow to the brain and nervous system, and enhances nerve cell function. Drug–herb interaction cautions
• Ginkgo biloba:
• plus aspirin: may induce spontaneous bleeding when combined with chronic use of aspirin. Increased bleeding potential reported after Ginkgo biloba usage in a chronic user (2 years) of aspirin.
• as noted above, however, individuals with MS should avoid the use of aspirin and other NSAIDs since these drugs inhibit the synthesis of myelinprotective anti-inflammatory prostaglandins obtained from omega-3 fats. Physical medicine
• Avoid excessive fatigue and marked temperature changes.
• Exercise is physically and psychologically helpful:
• in one study, MS patients were assigned to either an exercise or non-exercise group for 15 weeks. Aerobic training consisted of three 40 min sessions per week on a stationary bike that also had arm handles. The exercise group improved on all measures of physical function, social interaction, emotional behaviour, home management, total sickness impact profile score, and recreation.
• for spastic or severely weakened limbs, assisted movement and massage will improve circulation and may offer emotional and social benefits. ICIM Medics Approach If you feel that this article relates to you then please make an appointment to see one of ICIM Medics Natural Medical Practitioners. Some tests may be prescribed such as the ICIM Toxicity Assessment http://icimmedics.com/medical-assessments/toxicity-assessment/ depending upon your individual case, the results from these can be used by one of our Natural Medical Practitioners who will help you with your individualised treatment plan. This may include dietary, nutritional and/or botanical advice. This article is not meant to be used for treatment but for information purposes only. If you feel that this approach is appropriate for you please contact ICIM Medics on 045 844 819 or www.icim.ie e-mail : in**@ic**.ie Appointments can be arranged for you.

Disclaimer: These Wellness Protocols are not intended to replace the attention or advice of a physician or other qualified healthcare professional. These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure, or prevent any disease.
